Frequently Asked Questions
International Osteoporosis Foundation (IOF) believes FLS is the single most important thing that can be done to directly improve patient care and reduce spiralling fracture related healthcare costs worldwide. Fragility fractures are common; 1 in 2 women over 50 years of age will suffer one, as will 1 in 5 men. And a prior fracture doubles a patient’s future fracture risk.
With a globally aging population, fractures will continue to increase in numbers, while the cost incurred on governments will also spiral. IOF estimated in 2015 that the total direct cost of osteoporotic fractures in Europe to be 32 billion EUR per year, and projected that this will rise to 38.5 billion EUR by 2025.
Read more on the WOD 2012 report on the campaign
Many studies have demonstrated that FLS increases osteoporosis diagnosis, treatment initiation and adherence, while decreasing re-fracture and mortality rates.
IOF, through Capture the Fracture (CTF), calls on all hospitals and clinics, and governments around the globe to implement FLS.
Over 80% of fracture patients are never screened for osteoporosis, nor placed on treatment for the disease, despite the availability of effective medications that can significantly reduce future fracture risk.
This is why many patients go on to break another bone after the first fracture.
Most hospitals and clinics are failing to ‘capture’ the first fracture – which results in the patients to suffer from secondary fractures. Half of patients with hip fractures today have experienced prior fragility fractures in the past.
As a consequence, Capture the Fracture, an IOF initiative, was established in 2012 to narrow the secondary fracture gap – and – improve patient outcomes.
“The ‘Capture the Fracture® Partnership – Guidance for Policy Shaping’, with focus on the global need for Post-Fracture Care Coordination Programs, outlines the four simple building blocks of an effective policy response which has been shown to improve patient outcomes, deliver financial savings and save lives.
CTF recommends FLS to follow the internationally endorsed Best Practice Framework (BPF) to understand the essential and aspirational elements of the service model, and how to organize an effective, efficient service. Depending on the stage of development, and funding and resources available, the specific type of model an FLS should implement will differ. It is common for a FLS to begin by identifying only hip fracture patients, later incorporating other fracture types (non-hip patients, then outpatients and finally vertebral patients). A FLS also needs to decide whether it will be responsible for the entire patient pathway, from identification, investigation, treatment initiation to monitoring. In countries with established primary care infrastructure, the patient’s GP can be responsible for treatment initiation and monitoring. Please visit the CTF Resource Centre to find resources catered to FLS implementation.
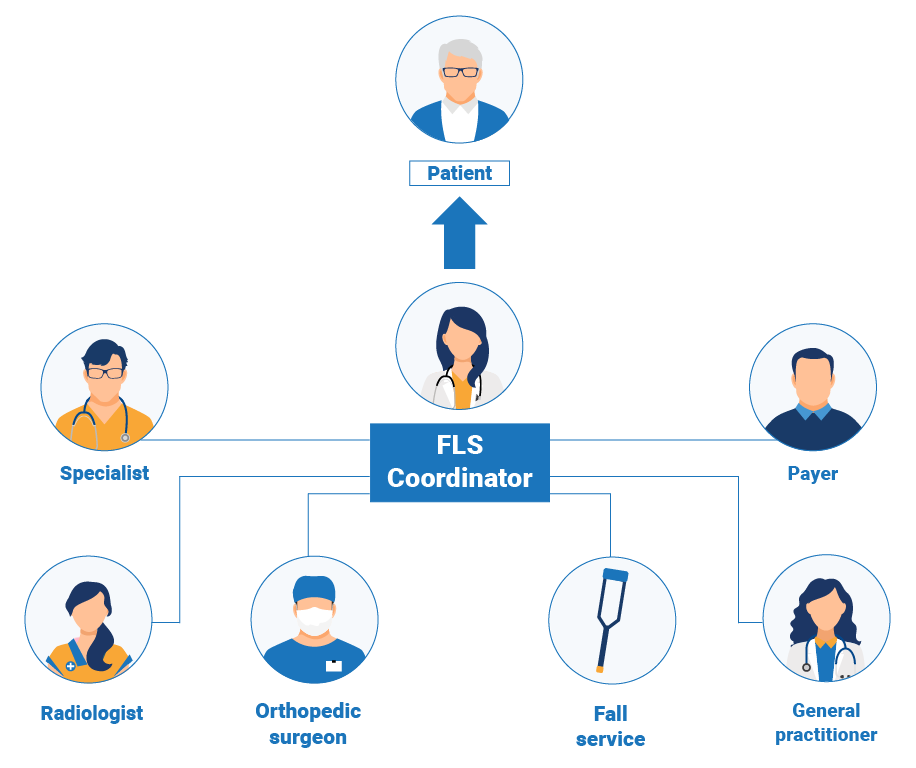
The FLS coordinator is a key member of the FLS team and can be any qualified health care professional. The coordinator is responsible for capturing patients with fragility fractures in the hospital or clinic, and ensuring that they are investigated, initiated on treatment and followed up. The coordinator plays a key role in ensuring the right patients are identified, but also in improving communication within the multidisciplinary FLS team and between physicians and patients. Learn more about FLS structure. Please view our webinar for more information on the role of the FLS coordinator.
CTF offers a variety of resources that serves as a good guide on how to implement a FLS. The International FLS toolkit is a comprehensive tool that makes a case for FLS and outlines the different steps for planning and developing FLS (used by health care professionals, hospital administrators, payers, policy makers). For hospitals and clinics who need more hands-on education and training on how they can implement FLS, the mentorship programme is available.
The Capture the Fracture® Resource Center contains resources on different key topics relevant to running an effective secondary fracture prevention service.”
In order to get mapped, FLS applicants must complete the BPF questionnaire . The CTF Steering Committee (SteerCo) will grade the service from both administrative and clinical perspectives which is determined by achievement against the BPF standards for four key fragility fracture patient groups - hip fractures, other in-patient fractures, outpatient fractures and vertebral fractures - and organizational characteristics. The FLS is given one of four ratings in each category - gold, silver, bronze or black. The scores of these five ratings are then used to determine the FLS’ overall rating - gold, silver or bronze. Read more on Best Practice Framework.
On average, from the day the FLS submits a questionnaire to the day the SteerCo provides a score report, takes approximately 3-4 months. The length will vary according to the volume of current applications, as well as the availability of the Steering Committee members.
We understand that your evaluation is important to you, and the IOF CTF team and SteerCo handles each application with utmost care. If you want to get in touch with us, please feel free to contact capturethefracture@osteoporosisfoundation
FLS is a care model that was first implemented in 1999 at the Western Infirmary and Southern General Hospitals in Glasgow. Since then many FLS have rolled out across the world, including very successful ones.
The CTF SteerCo is composed of experts who are leaders of some of the most successful FLSs in the world. Associate Professor Kassim Javaid, Co-Chair of SteerCo, leads the FLS at the Nuffield Orthopaedic Centre (NOC) in Oxford, whose team is supported by at least 4 full-time nurse practitioners. They identify at least 3000 patients a year, including hip fracture, inpatients, outpatients and vertebral fracture patients.
We advise you to consult the successful case studies’ page of the CTF website to learn more about these excellent services. https://www.capturethefracture.org/case-studies-successful-services
The benefits of joining the programme are numerous. Being mapped means having your FLS independently benchmarked against internationally agreed criteria and standards for secondary fracture prevention. The benchmarking also highlights areas of service delivery that are working well and spotlights areas for quality improvement.
CTF is a global platform with a vibrant community of experienced local and global FLS champions who can provide their expertise, mentoring and support for FLSs within the same country and internationally.
The map also provides visibility of FLS in your regional area for patients, health care professionals as well as for policymakers, underlining FLS’ commitment in the best management of patients with osteoporosis.
CTF’s key aim is to promote and help implementation of FLS globally. However, it also exists to be the global voice for secondary fracture prevention, and to drive policy changes internationally.